non-melanoma
Non- melanoma is a slow developing cancer that affect the upper layers of the skin. Basal Cell Carcinoma is a superficial (located on the surface) cancer that is slow growing and arises from keratinocytes. Metastasis (development to different region) is rare but local growth is destructive. It is the most common type of skin cancer. Squamous Cell Carcinoma is a malignant (harmful) tumour of cells- keratinocytes, that invades the tissue of the skin (dermis). This i9s the second most common type of skin cancer and can de developed from actinic keratoses.
-
Squamous cell carcinoma
Affects 1.8 million cases yearly in the United States [1]
The incidence increases with increased age
Rates of squamous cell carcinoma is higher in lighter- skinned people [2]
According to NICE guidelines, approx 25,000 cases are diagnosed each year
A full time GP is likely to diagnose at least 1 person every 1-2 years [3]
Basal cell carcinoma
Particularly common in white populations and in the US, the incidence has increased by more than 10% per year
The lifetime risk (risk of something occurring at some point in a lifetime) of basal cell carcinoma developing is 30% [4]
According to NICE, approx 75,000 cases of basal cell carcinoma are diagnosed each year
A full time GP is likely to diagnose at least one person with basal cell carcinoma per year. [3]
-
Overexposure to ultraviolet light from the skin/artificial tanning beds and sunlamps [1]
-
Medical Students
UV Radiation Exposure
UV radiation (mainly UVB) damages skin cell DNA
Leads to mutations that can initiate carcinogenesis
DNA Damage and Mutations
UV light forms pyrimidine dimers in DNA
Inadequate repair causes accumulation of mutations over time
Loss of Cell Cycle Control
Mutations in tumour suppressor genes and oncogenes disrupt normal regulation
Results in uncontrolled cell proliferation
Inactivation of Tumour Suppressor Genes
Key genes like TP53 (p53) and PTCH1 lose function
Impairs DNA repair and apoptosis, allowing malignant cells to survive
Activation of Oncogenes
Oncogenes (e.g. RAS) become constitutively active
Drive continuous and abnormal cell growth
Chronic Inflammation
Prolonged UV exposure triggers inflammatory mediators and cytokines
Promotes tumour development and impairs immune surveillance
Immune Evasion
Tumour cells evade detection and elimination by the immune system
Enables persistence and growth of malignant cells
Angiogenesis
Tumours stimulate formation of new blood vessels
Ensures oxygen and nutrient supply for sustained growth
Invasion and Metastasis
Cancer cells infiltrate dermal and subcutaneous tissues
Rarely, spread via lymphatics or bloodstream to distant organs (less common than in melanoma)
Patients
Sun and Tanning Exposure (UV Radiation)
Too much time in the sun or using tanning beds exposes the skin to harmful ultraviolet (UV) rays
These rays can damage the DNA in skin cells, which may lead to cancer over time
DNA Damage in Skin Cells
UV rays can cause changes in the structure of DNA inside skin cells
If these changes aren’t fixed, they build up and increase the risk of cancer
Loss of Control Over Cell Growth
Some DNA changes affect how cells grow and divide
This can lead to uncontrolled cell growth and formation of cancer
Weakened Natural Defences (Tumour Suppressor Genes)
Our bodies have genes that usually stop tumours from forming
If these genes are damaged, they can no longer stop harmful cells from growing
Overactive Cell Growth Genes (Oncogenes)
Some genes that control normal cell growth may become overactive
This can push cells to divide too quickly and form tumours
Long-Term Inflammation
Ongoing skin damage and inflammation from UV rays can help cancer cells grow
Inflammation also makes it harder for the body to remove abnormal cells
Escaping the Immune System
Cancer cells can sometimes avoid being detected by the immune system
This allows them to grow and spread more easily
New Blood Vessels for Tumours (Angiogenesis)
As cancer grows, it creates new blood vessels to get more oxygen and nutrients
Spread to Other Areas (Invasion and Metastasis)
In rare cases, non-melanoma skin cancer can spread to deeper skin layers or other parts of the body
This is less common compared to melanoma [5]
-
History of non-melanoma/ skin cancer
Pale skin
Large number of moles/freckles
Suppressed immune system caused by medication
Weakened immune system with co-existing medical conditions
Older age
Blue eyes or blonde/red hair
Exposure to certain chemicals [6,7]
-
Basal cell carcinoma
Open sores that bleed/ooze/crust
Redness
Raised patches
Crusting or itching of the affected skin
Pink/red/pearly-white bump
White/yellow/waxy areas
Poorly defined borders
Squamous cell carcinoma
Wart-like growth
Scaly appearance of the skin
Irregular/poorly defined borders
Open sores
Raised growth
Rough surface with central dip (depression) [8]
-
Biopsy
A small procedure where a sample of all of the tumour is taken from the skin to be studied under the microscope
This usually takes several weeks before results are available
Further tests such as lymph node examination may be required
Used to assess whether the cancer has spread
Fine needle aspiration
In a case of concerns about cancer spreading, may be needed to do a biopsy on a lymph node [6]
-
Psoriasis
Seborrheic keratoses- non cancerous skin growth
Sebaceous hyperplasia- growth of sebaceous glands (glands that grow near hair follicles)
Nevus (mole)
Cherry angioma- overgrowth of blood vessels that create cherry red bumps [9]
-
Medical Students
Multidisciplinary Team (MDT):
Involves dermatologists, surgeons, plastic surgeons, radiation oncologists, and medical oncologists
Other professionals: physician associates, nurse practitioners, nurses, social workers, pharmacists, counsellors, dieticians
Treatment decisions depend on:
Tumour size, type, location
Side effects and patient preferences
Overall health and shared decision-making
Common treatment options:
Surgery
Mainstay of treatment
Involves excision of tumour and surrounding margins
Choice of procedure depends on tumour characteristics
Radiation Therapy
High-energy rays destroy cancer cells
Delivered externally or via brachytherapy
Used alone or post-surgery, especially with lymph node involvement
Other Local Treatments
Photodynamic therapy (PDT)
Cryotherapy
Laser therapy for superficial or precancerous lesions
Medications (Systemic or Local):
Topical Chemotherapy: for superficial cancers
Targeted Therapy: vismodegib, sonidegib for advanced BCC
Immunotherapy: cemiplimab, pembrolizumab, avelumab, retifanlimab
Patients
Your care team will include many specialists working together:
Skin doctors (dermatologists), cancer doctors (oncologists), surgeons, and other experts
Nurses, pharmacists, social workers, counsellors, and dieticians also support your treatment
Treatment decisions are made together with your doctor, considering:
Size and location of the cancer
Your health and what matters most to you
Possible side effects of treatment
Common treatments for non-melanoma skin cancer:
Surgery
Most common treatment
Removes the cancer and a small border of healthy skin
Radiation Therapy
Uses strong energy rays to kill cancer
Can be done from outside the body or placed inside
Used instead of or after surgery in some cases
Local Treatments
Photodynamic therapy: light-based treatment that kills cancer cells
Cryotherapy: freezes cancer cells
Laser therapy: uses focused light to remove early skin cancers
Medication Treatments
Medicines applied to the skin or taken by mouth
Chemotherapy creams
Targeted drugs like vismodegib or sonidegib for advanced skin cancer
Immunotherapy drugs like cemiplimab or pembrolizumab help the immune system fight cancer
-
Scarring after treatment
Hyper/ hypo-pigmentation at sites of treatment
Tightness and skin texture change due to radiation therapy
Lymphedema- swelling of the lymphatic system, leads to fluid buildup
Wound infection after surgery
Hemeatoma- bleeding under the surface of the skin
Numbness and pain of the sites of treatment
Damage to the muscles/nerves/bones due to untreated cancer
Metastasis- cancer can return and develop to another part od the body
Mental health (anxiety and depression) caused by diagnosis and potentially due to treatment [10]
-
Darker skinned people don’t get skin cancer
Only sun exposure can cause skin cancer
Only older people get skin cancer
High SPF sunscreen completely protects you from skin cancer
Tanning beds don’t pose as a risk for skin cancer
You don’t need to wear sunscreen in winter or cloudy days [11]
-
What is the process of investigating skin patches/areas of concern?
Will removing the skin cancer be effective as a single form of treatment?
How do I determine the stage of cancer?
What can I do to prevent the skin cancer spreading?
How can I manage any complications of my skin cancer?
What follow-up support can I get during and after treatment?
-
Macmillan Cancer Support
Cancer.net
NHS Inform
-
[2]https://wiki.cancer.org.au/australia/Guidelines:Keratinocyte_carcinoma/Epidemiology_SCC
[3] https://cks.nice.org.uk/topics/skin-cancers-recognition-referral/background-information/prevalence/
[5] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4307792/
[6] https://www.nhs.uk/conditions/non-melanoma-skin-cancer/
[8] https://www.cancer.net/cancer-types/skin-cancer-non-melanoma/symptoms-and-signs
[9] https://sundoctors.com.au/blog/top-5-conditions-often-mistaken-skin-cancer/
[10] https://www.everydayhealth.com/skin-cancer/complications/
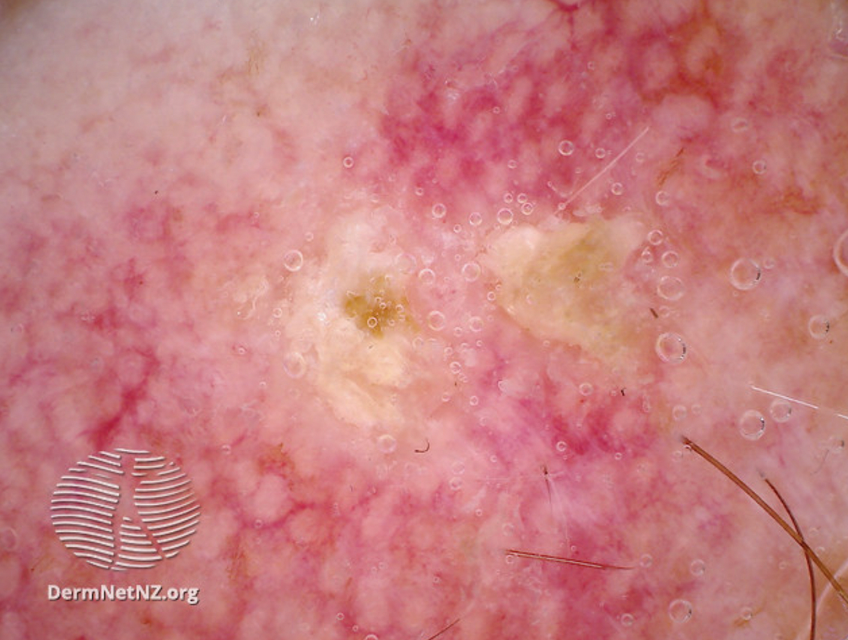
Source: DermNetNZ.org
Non-melanoma
Pigmented basal cell carcinoma seen with a dermoscopy (used to examine the skin)
Source: DermNetNZ.org
Non-melanoma
Dermoscopic image of actinic keratosis
Source: Atlas of Black Skin
Non-melanoma
Raised white lesion seen in squamous cell carcinoma
Source: Atlas of Black Skin
Non-melanoma
Pigmented basal cell carcinoma
Source: DermNetNZ.org
Non-melanoma
Basal cell carcinoma affecting the face
Source: Waikato District Health Board; DermNetNZ
Non-melanoma
Squamous cell carcinoma on the cheek
Source: Atlas of Black Skin
Non-melanoma
Pigmented basal cell carcinoma
Actinic Keratosis
Actinic keratoses are precancerous (small chance of developing into cancer) patches of skin (that are likely to be exposed to the sun. eg. face, hands) that change due to frequent and long term exposure to the sun. This condition affects the skin cells- known as keratinocytes. It has a chance of progression into squamous cell carcinoma but ranges from less than 1 to 10% in likelihood of progression.
-
People with fair skin are most likely to develop actinic keratoses according to studies conducted in Australia, Northern Europe and the US [1]
NICE estimates that over 23% of the population in the UK aged 60 and above have actinic keratosis [2]
The WHO have estimated that the highest levels are observed in Caucasians living close to the Equator [3]
A study, carried out in Austria, found a prevalence of actinic keratoses of 31% of patients over 30 years old.
The prevalence was also higher in men than in women and increased with age [4]
-
Damage to the skin caused by UV (ultraviolet light) from exposure to:
Tanning beds
The sun [6]
-
See above pathophysiology [5]
-
Exposure of UV rays from the sun or tanning beds
People with pale skin
People with blonde/red hair
People with blue/green/grey eyes
Increased age
Weakened immune systems (eg. AIDS, organ transplant etc)
Rare conditions that cause hypersensitivity to UV rays (eg. albinism- no melanin, xeroderma pigmentosum- condition causing increased reactions/sensitivity to the sun) [7]
-
Scaly patches found on areas of the skin
Some can form a horn shaped growth
Thickened skin
Pigmentation change to pink, red, grey or brown
Roughness
Raised spots
Dryness [6]
-
Clinical assessment based on presenting symptoms and appearance of patches
Dermoscopy is an exam of the skin using skin surface microscopes to assess the areas of concern
Biopsy (a sample of the skin is taken) is necessary to exclude differential diagnosis such as squamous cell carcinoma [8]
-
Seborrheic keratosis (dandruff)
Squamous cell carcinoma- type of skin cancer that affects the sqaumous cells
Bowen’s disease- an early form of squamous cell carcinoma
Solar lentigo- harmless patch of darkened skin
Stucco keratosis- multiple harmless wart like lesions (sores) typically small with a stuck on appearance
Basal cell carcinoma- type of skin cancer that affects the basal cells
Porokeratosis- abnormal keratinisation (process where skin cells form and produce keratin) with ridge-like borders on the skin
Clear cell acanthoma- a rare, non-cancerous skin tumour
Psoriasis- skin condition that causes dry, flaky patches of skin
Lupus erythematosus- disease where the immune system attacks the body’s tissues, causing inflammation and damage to the skin
Lichen planus- a condition that is non-infectious and causes an itchy rash that affects many areas of the body
Viral warts- a common, non-cancerous condition that causes regions of damage through infection [9]
-
Medical Students
Topical Therapies:
3% Diclofenac – NSAID used for actinic keratosis; anti-inflammatory and anti-proliferative
5% Fluorouracil (5-FU) – Antimetabolite interfering with DNA synthesis in precancerous/cancerous cells
5% Imiquimod – Immune response modifier stimulating interferon and cytokine production
0.5% 5-FU + 10% Salicylic acid – Combination enhances penetration and keratolysis
3.75% Imiquimod – Lower-concentration regimen for broader field application
Other Therapies:
Liquid Nitrogen (Cryotherapy) – Freezes and destroys abnormal skin cells
Curettage – Scraping off superficial skin lesions, often followed by cautery
Patients
Cream or Gel Treatments (Topical Therapies):
3% Diclofenac – A gel that reduces inflammation and helps remove damaged skin
5% Fluorouracil (5-FU) – A cream that kills abnormal skin cells
5% Imiquimod – A cream that boosts your immune system to fight skin damage
0.5% 5-FU + 10% Salicylic acid – A combo treatment that helps peel away damaged layers
3.75% Imiquimod – A gentler version used over larger areas of skin
Other Skin Treatments:
Liquid Nitrogen – Freezes and destroys abnormal skin areas
Curettage – Scraping away damaged or abnormal skin, sometimes followed by heat to stop bleeding [12]
-
Risk of developing into squamous cell carcinoma
Cutaneous horn (bone structure with keratin) formation
Actinic cheilitis- lip involvement with actinic keratosis
Basal cell carcinoma- type of skin cancer that affects the basal cells
Melanoma- a cancerous skin condition that affects the melanocytes
Rare forms of skin cancer such as Merkel cell carcinoma [8]
-
Actinic keratoses always turns into squamous cell carcinoma
Actinic keratoses does not require treatment
Actinic keratoses is cancerous [10,11]
-
How can I tell if my patches change/ develop?
How can I prevent actinic keratoses developing in everyday activities?
How long does treatment take to be effective?
What is the process of investigating actinic keratoses?
What happens if I don’t treat actinic keratosis?
-
British Associaion of Dermatologists
The Skin Cancer Foundation
Sussex Community Dermatology Service
-
[1] https://www.uptodate.com/contents/epidemiology-natural-history-and-diagnosis-of-actinic-keratosis
[2] https://www.pcds.org.uk/clinical-guidance/actinic-keratosis-syn-solar-keratosis#:~:text=An
[3] https://apps.who.int/iris/bitstream/handle/10665/43505/9241594403_eng.pdf
[4] https://academic.oup.com/bjd/article-abstract/171/6/1415/6616338
[5] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4307792/
[6] https://www.aad.org/public/diseases/skin-cancer/actinic-keratosis-causes
[7] https://www.hopkinsmedicine.org/health/conditions-and-diseases/actinic-keratosis#:~:text=
[8] https://dermnetnz.org/topics/actinic-keratosis
[9] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6939186/#:~:text=Differential
[11] https://www.skincancer.org/blog/is-actinic-keratosis-skin-cancer/
[12] https://www.pcds.org.uk/files/general/AK_guidelines_2020-new-web-v01.pdf